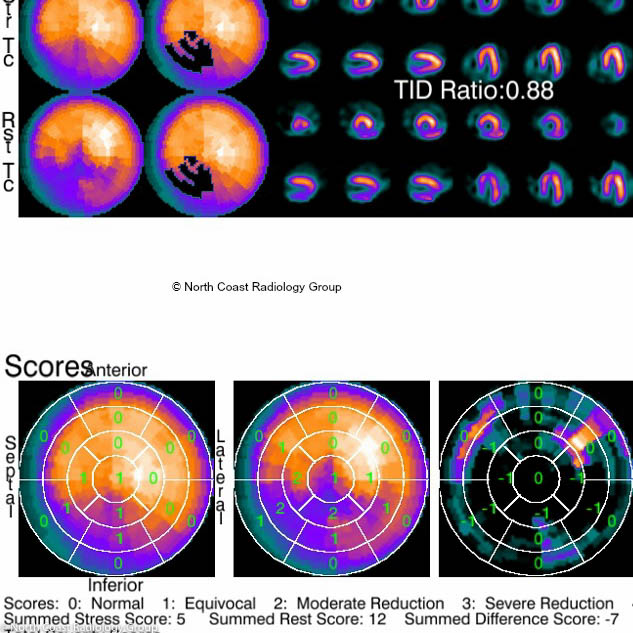
Nuclear Medicine is the branch of radiology that uses radioactive materials to determine if certain organs such as the heart, kidneys, liver, thyroid, brain and lungs are functioning properly. It is also used to examine the bones for cancer, infection or trauma.
Nuclear medicine uses very small amounts of low-level radioactive chemicals, called radiopharmaceuticals, which are introduced into the body either intravenously or orally. Radiopharmaceuticals are specially formulated to be collected temporarily in the specific part of the body to be studied.
Nuclear medicine imaging procedures often identify abnormalities very early in the progression of a disease, sometimes long before problems are apparent with other diagnostic tests
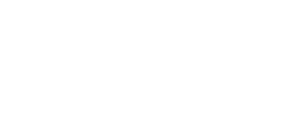
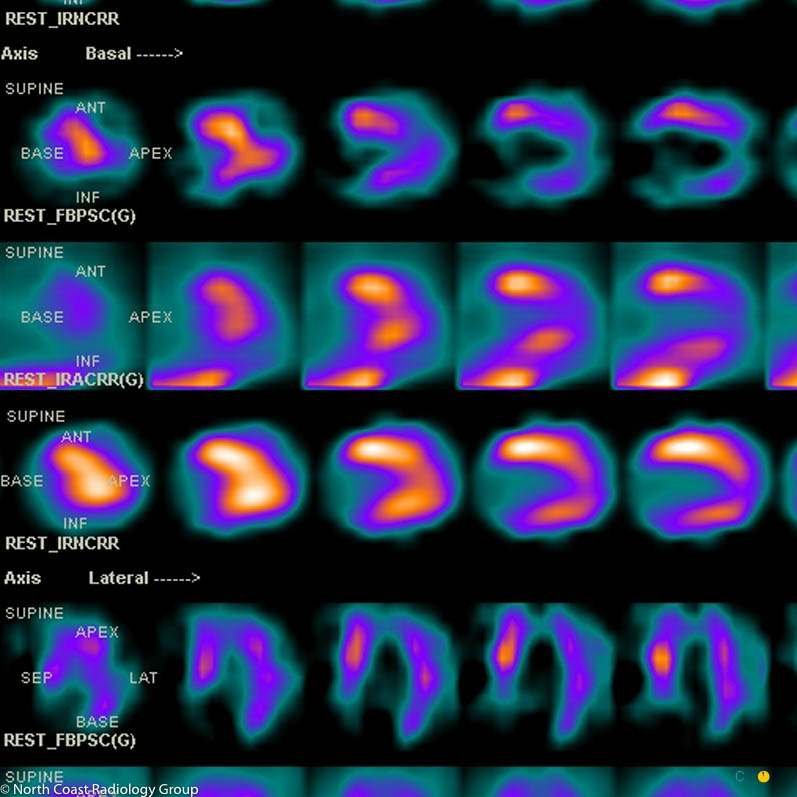
Spect CT
Single-photon emission computed tomography (SPECT CT) is a non-invasive nuclear medicine test that enables doctors to evaluate disease based on functional and metabolic information. SPECT CT uses a gamma camera just like conventional nuclear medicine (2D images), but creates cross-sectional slices that can be reconstructed into 3D information.
The gamma camera is rotated around the patient through a full 360° while projections are acquired typically every 3–6°.
SPECT CT uses the x-ray attenuation information from computed tomography to correct for SPECT attenuation, which is important for accurate 3D signal measurement.
In addition, SPECT CT provides more anatomical images that precisely localise disease, which improves sensitivity and specificity. SPECT CT has proven to be valuable in oncology for identifying metastatic cancer.
The combined image SPECT CT enables the radiologist who analyses the scan to pinpoint the site of any abnormality more accurately. In complex bony areas such as the spine or feet, determining exactly which bone is affected on 2D nuclear medicine scans is challenging. Combining SPECT and CT provides essential anatomical mapping to allow precise localisation in 3D.